What can I expect after treatment?
If vision is present or there is a chance vision will return:
Cyclocryocoagulation (CCC) or Transscleral Diode Laser Cyclophotocoagulation (CPC)
Cryotherapy or a diode laser is used to destroy cells of the ciliary body, which is the gland located inside of the eye that produces fluid. This procedure is estimated to control eye pressure in 60-70% of patients for a period of 6 months. Complications include pressure spikes, bleeding, and corneal ulcers. The cryotherapy or the laser surgery is non-invasive (laser energy is delivered by a laser or cryo probe placed on the surface of the eye; however a short episode of general anesthesia is required to perform the procedure. Most pets must stay in the hospital for pressure monitoring for 1 to 3 days after laser or cryo surgery.

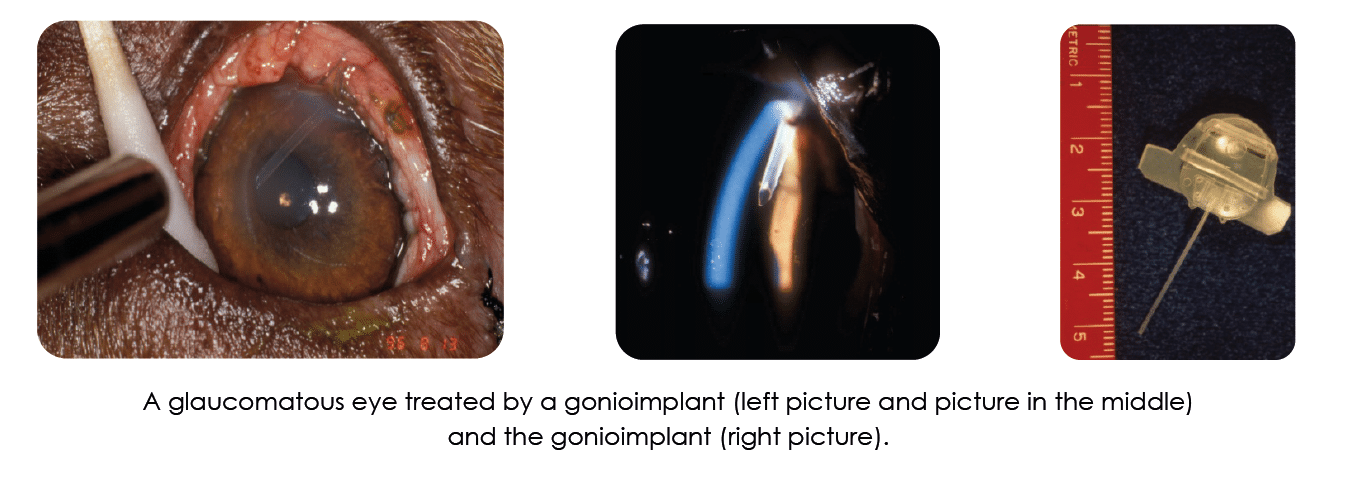
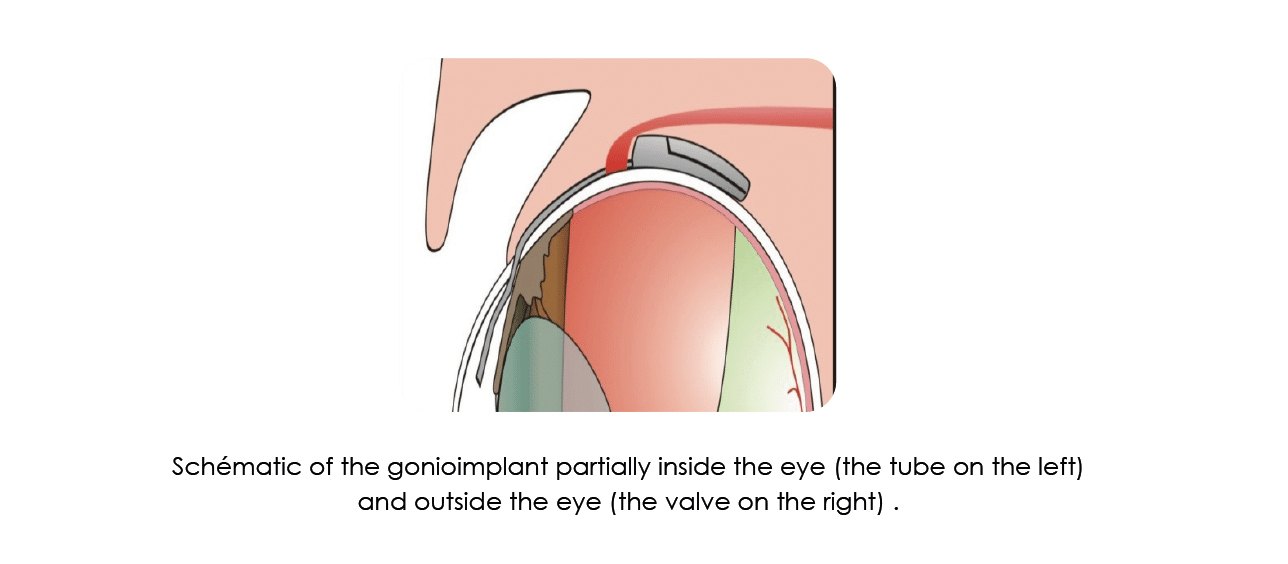
Aqueous shunt implant (gonioimplant)
A small tube is implanted inside the eye. This tube, or shunt, sits partially inside the eye and partially outside the eye under the mucous membrane (conjunctiva) around the eye to allow fluid to leave the eye when pressure increases above a specific level. The success rate for this procedure to control pressure is similar to laser surgery. When laser treatment or cryotherapy is combined with placement of a gonioimplant, the estimated success rate per eye is maximized. Complications include scarring around the shunt causing back-up of the fluid in the eye and dislocation of the shunt. General anesthesia is required along with overnight monitoring.
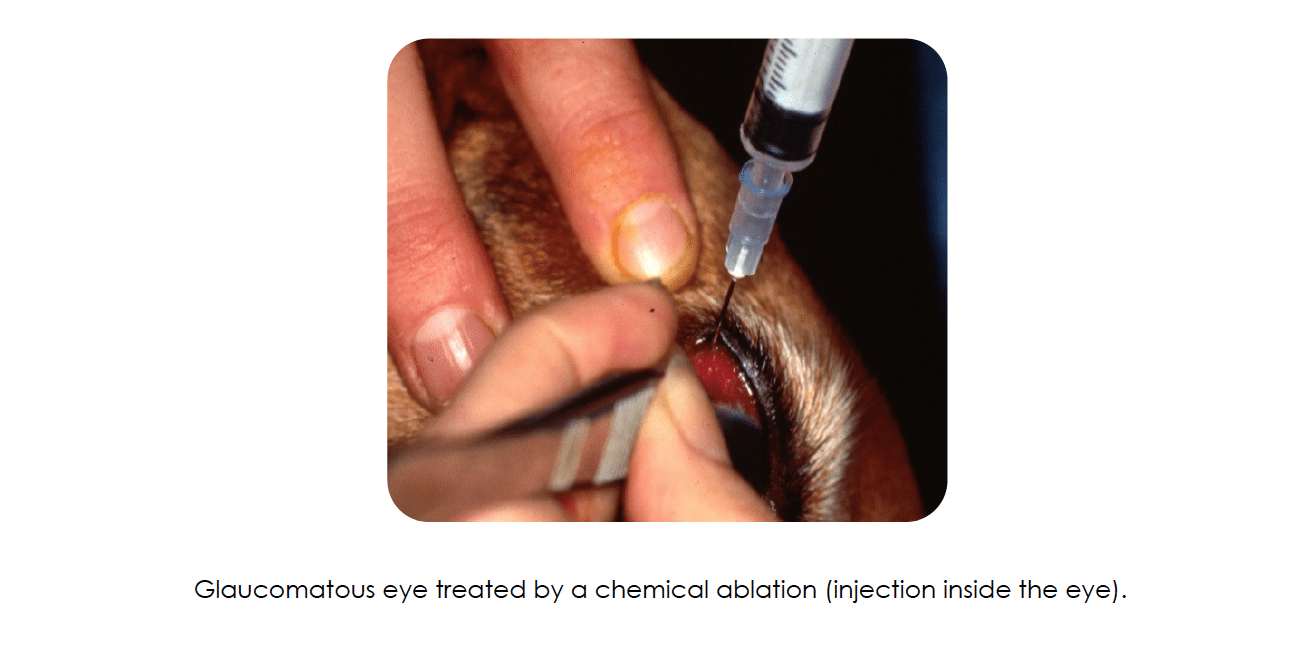
Ciliary Body Ablation (CBA) by Injection
This procedure is most often performed on geriatric patients or patients with a higher anesthetic risk (such as those with cardiac or metabolic conditions). The patient is given either a strong sedative or placed under brief general anesthesia (5-10 minutes). During this procedure, a combination of an antibiotic and cortisone is injected into the eye. These medications destroy a significant portion of the ciliary body which is the gland inside the eye that produces fluid (aqueous humor). This will permanently decrease the amount of fluid produced inside the eye, thereby reducing pressure. The procedure is successful in 80-90% of patients, depending on the form of glaucoma. Should the eye pressure remain elevated 6 weeks following the procedure, a second injection may be recommended. All patients will be treated with a topical cortisone medication for a period of several weeks following the injection and some require long term, lowfrequency treatment to maintain eye comfort. Many eyes following injection become smaller in size, although this is not uncomfortable or often dramatic. Other potential complications include bleeding within the eye (usually associated with a retinal detachment), chronic inflammation and corneal ulcer.
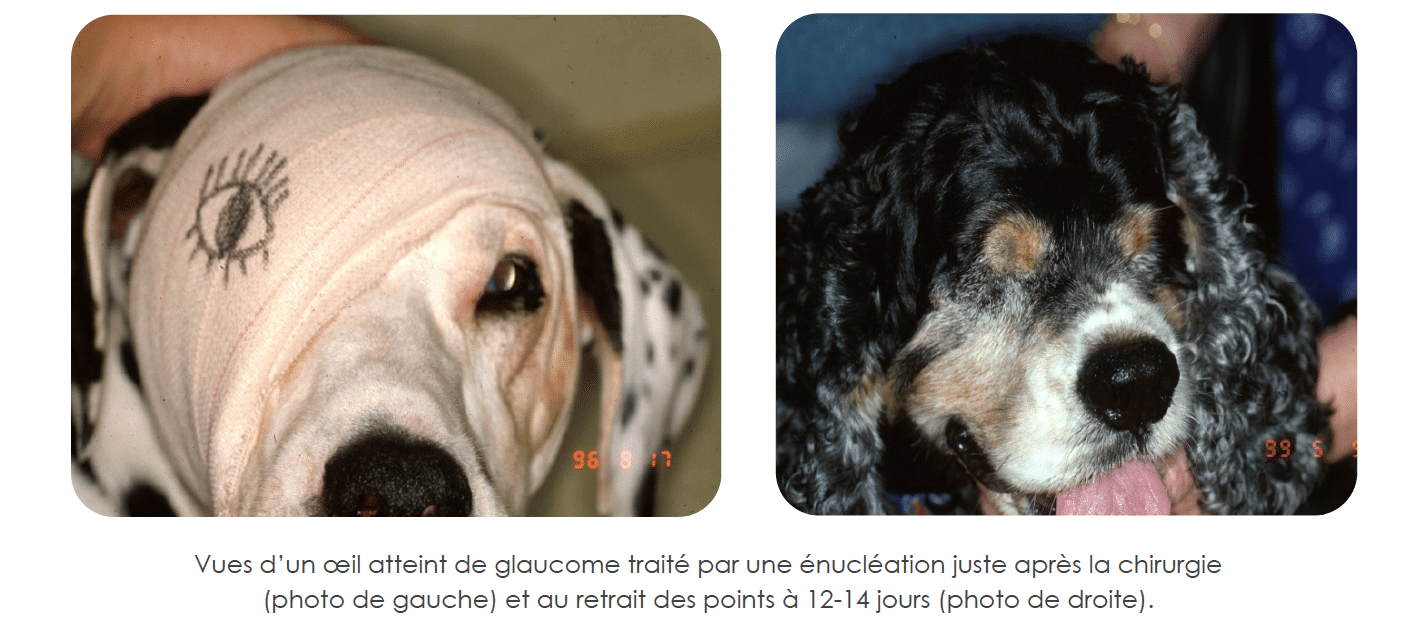
Enucleation (eye removal)
The eye is removed and the eyelids are permanently closed. Provided there is not an infection or cancer present within the orbit, a silicone implant is may be placed in the eye socket to prevent a sunken appearance. General anesthesia is required. This procedure rarely requires overnight hospitalization. Immediately following surgery you can expect to see some swelling and minor bruising around the surgical site. Oral antibiotics and pain medications will be given for the first week. Sutures are removed after 10 to 14 days when the incision has healed. While the risk is low, there is a potential for infection to develop around the orbital implant despite prophylactic treatment with antibiotics. Should an infection develop, a second surgery would likely be necessary to remove the prosthesis.
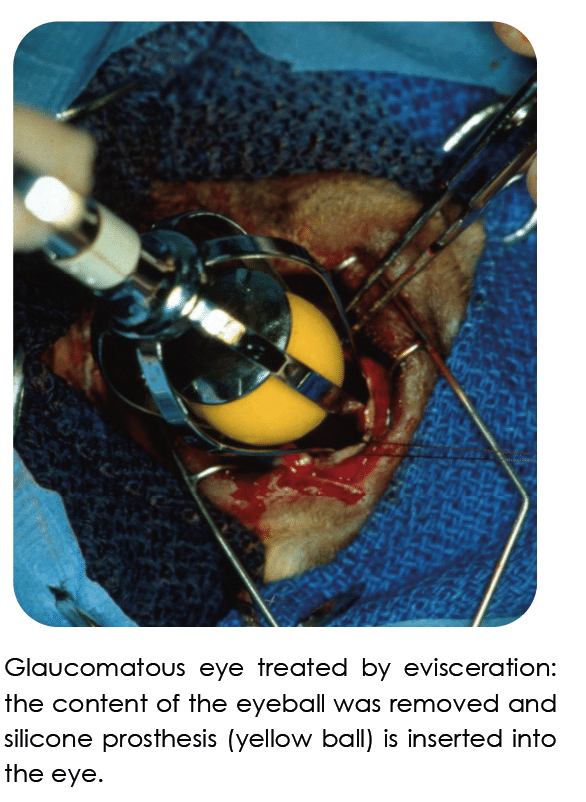
Evisceration with Intrascleral Prosthesise
This surgical procedure provides a cosmetic alternative to enucleation. In order to be a candidate for the surgery, the eye must have normal tear production and have a healthy cornea. The surgery involves making an incision through the conjunctiva and sclera (the white shell of the eye) and removing the contents within the eye. A silicone sphere (prosthesis) is then placed within the eye, and the conjunctiva and sclera are sutured closed. The eyelids are also partially closed (temporarily) to protect the surgical incision. A few days later the eyelid sutures are removed. The patient has what appears to be a completely functional though non-visual eye. They are able to move the eye and blink as before. Postoperative therapy includes oral and topical antibiotics and an oral anti-inflammatory / analgesic for 1 week, and use of an Elizabethan collar. After the eyelid sutures are removed most patients are then treated with a topical cortisone medication to reduce any remaining surgical or pre-existing inflammation for 2-4 weeks. Many corneas develop a cloudy or bluish haze during the healing process, some of which may be permanent. Patients with intrascleral prostheses will usually require routine lifelong care to maintain optimal corneal health. Long-term topical therapy includes lubricating eye drops, gels or ointments applied 2-3 times daily. Some patients experience a decline in tear production (dry eye syndrome) months to years following surgery and require topical medications to stimulate tearing. It is important to be aware that these patients can accidentally injure their corneas and require treatment